OMSSA is featuring several 2024 Local Municipal Champion award recipients and their work in the Knowledge Exchange Blog. Please read this entry from the County of Simcoe and Orillia Soldiers’ Memorial Hospital below.
In the heart of Simcoe County, during a time of ongoing COVID-19 Pandemic response, a transformative partnership emerged between the County of Simcoe Ontario Works Division and Orillia Soldiers’ Memorial Hospital (OSMH). This collaboration was born out of urgency as an innovative opportunity to support our vulnerable populations, including those experiencing homelessness, and unattached patients in the community, aiming to increase access to care in the right place, outside of the emergency department. This blog post delves into the innovative strategies and tangible benefits of this partnership, highlighting how it has significantly improved health outcomes and set a precedent for integrated human services.
 |
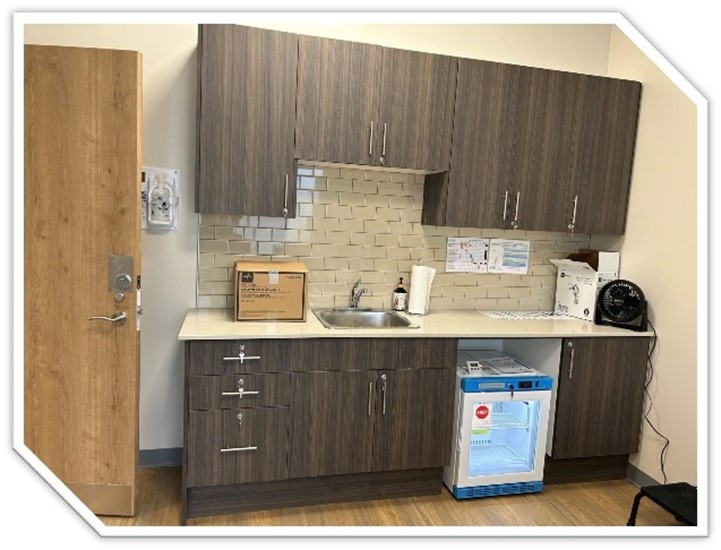 |
The Genesis of a Centralized Care Clinic
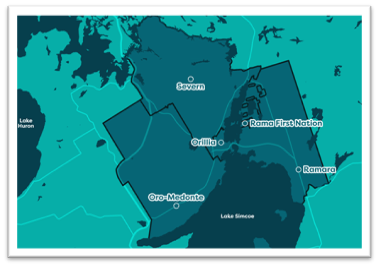 The County of Simcoe’s leadership team, recognizing the pressing need for accessible healthcare, supported OSMH in creating a centralized Care Clinic, in a community of a higher urban than rural mix. The clinic, originally opened as the central COVID-19 assessment centre for the community, evolved into a space to serve the approximate 20,000 (or 22%) unattached patients in the community who had no access to primary care outside of the one local emergency department. The goal was clear: to keep these patients out of the emergency department and ensure they received the care they needed in the right care setting.
The County of Simcoe’s leadership team, recognizing the pressing need for accessible healthcare, supported OSMH in creating a centralized Care Clinic, in a community of a higher urban than rural mix. The clinic, originally opened as the central COVID-19 assessment centre for the community, evolved into a space to serve the approximate 20,000 (or 22%) unattached patients in the community who had no access to primary care outside of the one local emergency department. The goal was clear: to keep these patients out of the emergency department and ensure they received the care they needed in the right care setting.
The centralized Care Clinic is a testament to the power of community partnership, innovation and community collaboration. By evolving the model borne out of the pandemic, pooling resources and expertise, the County and OSMH had created a proof of concept for the province that offered comprehensive care to those who needed it most, while awaiting attachment to a primary care provider. This initiative not only alleviated the burden on emergency services but also provided a more sustainable and effective healthcare solution for the community in alignment with the Province’s Your Health initiative, A Plan for Connected and Convenient Care, and the newly formed Provincial Primary Care Action Team (2024), investing $1.8B to connect Ontarians to a Family Doctor and Primary Care Team by 2029.
“The County of Simcoe Social & Community Services Health Care Clinic is deeply connected to Orillia’s community, strengthening by the key connection between primary care and social services. By providing accessible, comprehensive care, the clinic has created a space where there is positive and significant impact on vulnerable populations. As a nurse practitioner and primary care provider at the clinic, I see firsthand how our work impacts both individual, families and the community.”
Malcolm Morum, RN, BScN, MHScN, NP-PHC
Executive Director/Nurse Practitioner
Huronia Nurse Practitioner-Led Clinic
Tangible Benefits and Improved Health Outcomes
 The benefits of this partnership were evident in the improved health outcomes for the community. Vulnerable clients were able to experience better access to primary care, more comprehensive support, and a more responsive and efficient health system to serve them outside of the local Emergency Department, including in community spaces (local Shelter and Ontario Works offices directly).
The benefits of this partnership were evident in the improved health outcomes for the community. Vulnerable clients were able to experience better access to primary care, more comprehensive support, and a more responsive and efficient health system to serve them outside of the local Emergency Department, including in community spaces (local Shelter and Ontario Works offices directly).
The centralized Care Clinic had become a lifeline for over 1,700 unique patients in our region, offering services that addressed both immediate health concerns and chronic disease management.
One of the most significant impacts had been the reduction in emergency department visits. By providing a dedicated space for unattached patients to receive care, the clinic had helped to divert non-emergency cases away from the hospital’s emergency department. This not only reduced wait times and pressure on emergency services but also ensured that patients receive the appropriate level of care for their needs; allowing for follow-up and care continuity that is not offered through a visit to the emergency department. Ultimately, this innovative partnership and care model was awarded $2.3M in provincial funding to sustain the model forward.
Leadership and Innovation in Service Delivery
 The leadership of the County of Simcoe Ontario Works team played a pivotal role in bridging gaps in service delivery in a highly innovative manner. Their efforts have set a precedent for how the municipal sector can significantly enhance community health and well-being. By working closely with OSMH and other partners like the Huronia Nurse Practitioner Led Clinic and the Couchiching Ontario Health Team (OHT), they have created a seamless network of support that ensures vulnerable individuals receive the care they need.
The leadership of the County of Simcoe Ontario Works team played a pivotal role in bridging gaps in service delivery in a highly innovative manner. Their efforts have set a precedent for how the municipal sector can significantly enhance community health and well-being. By working closely with OSMH and other partners like the Huronia Nurse Practitioner Led Clinic and the Couchiching Ontario Health Team (OHT), they have created a seamless network of support that ensures vulnerable individuals receive the care they need.
With renewed funding now established, a key innovation has been the strategic use of centralized and decentralized spaces across municipal and health service organizations, such as the local community shelter and direct space within Ontario Works offices for integrated client access. This model has allowed for the delivery of health and social services directly to vulnerable and underserved clients and patients.
Since its inception in July 2024, that clinic has served over 1,000 unique individuals – many who are recipients of Ontario’s social assistance programs. This approach has eliminated the need for vulnerable individuals to navigate multiple, often fragmented, services on their own; notably in a rural community without any walk-in clinics. Instead, clients now receive comprehensive support in a familiar and accessible environment, fostering better engagement and outcomes.
When I first heard about the clinic coming into the office, I was ecstatic to hear that health care was going to be more accessible for our clients. It was not too long after that I had a client that could benefit from this service. My client came to the office, feeling quite defeated about a future path. He wanted to apply for ODSP but did not have a family doctor who could support this process and did not know where to turn from there. I was able to let him know about Malcolm and his team and that although it might not be a one stop shop to getting the package competed, he might find himself benefitting from what was to come.
My client has been consistently working with the HNPLC now for several months, they have sent him for MRI’s, completed paperwork, done blood work and continue to follow up with him on other health needs, helped him to access pain clinics close to home, etc. This client has been suffering for many years with chronic back and leg problems, and this has gone undiagnosed, and he is now starting to gain more knowledge about his health and his health journey. I have been thanked many times for the support this clinic has given him and continue to give my thanks to Malcolm and all the NP’s that support this wonderful program.
Laura Alford
Ontario Works Caseworker
County of Simcoe
The Ontario Works team has also significantly advanced local health and social service management through their ongoing integrated partnership with the Couchiching OHT. By collaborating around clients and patients, they have ensured that support is delivered in a manner that promotes success and well-being in a sustainable manner. This integrated approach has been instrumental in creating a more responsive and efficient health system that meets the needs of the community and ongoing opportunities to design healthcare delivery, such as the introduction of counselling services to this integrated model.
From its inception, the County of Simcoe Social & Community Services Health Care Clinic, has brought primary health care right to those who truly need it. Not only does the clinic provide acute health care, but they bring a compassionate and comprehensive approach to patient care, supporting access to additional community supports, mental health support, along with supporting individuals with social assistance related forms and processes. Observing the collaborative efforts between Nurse Practitioners and caseworkers, all working towards the shared goal of supporting community members through a holistic and person-centred approach, is truly inspiring. With the planned enhancements to our service model, I am incredibly excited to witness the ongoing positive impact on our community, particularly for its most vulnerable members.
Amy Marshall
Acting Director, Community Support & Wellbeing
County of Simcoe
A Model for Integrated Human Services
 The partnership between the County of Simcoe Ontario Works Division and OSMH serves as a model for integrated human services and integrated governance. It demonstrates how collaboration and innovation can lead to significant improvements in community health and well-being. By breaking down silos and working together, these organizations have created a system that is more than the sum of its parts.
The partnership between the County of Simcoe Ontario Works Division and OSMH serves as a model for integrated human services and integrated governance. It demonstrates how collaboration and innovation can lead to significant improvements in community health and well-being. By breaking down silos and working together, these organizations have created a system that is more than the sum of its parts.
In parallel to this local partnership, the Ontario Hospital Association (2024) recently published a report on Projected Patterns of Illness in Ontario, truly calling for innovation and partnerships such as these, in order to reimagine healthcare delivery in a manner that will be able to support our growth and aging populations.
The original proof of concept for this partnership, the centralized Care Clinic, was a shining example of what could be achieved when organizations come together with a shared vision. It proved to be the blueprint for other communities looking to improve access to care and support for vulnerable populations and allowed for permanent base funding for primary care expansion to be awarded to our community. The success of this initiative underscores the importance of integrated human services and the positive impact they can have on individuals and communities.
Conclusion
The partnership between the County of Simcoe Ontario Works Division and the Orillia Soldiers’ Memorial Hospital is a testament to the power of collaboration, partnership and innovation in healthcare. By creating a centralized Care Clinic and leveraging the strengths of each organization, these partners have significantly improved access to care for vulnerable, underhoused, and unattached patients in the community. The tangible benefits of this innovative partnership are evident in the improved health outcomes and quality of life for patients. This partnership serves as a model for other communities looking to improve access to care and support for vulnerable populations. It highlights the importance of integrated human services and the positive impact they can have on individuals and communities. By working together, we can create a healthier, more equitable future for all.


